Building a Resilient Mental Health Ecosystem: Strategy and Opportunity
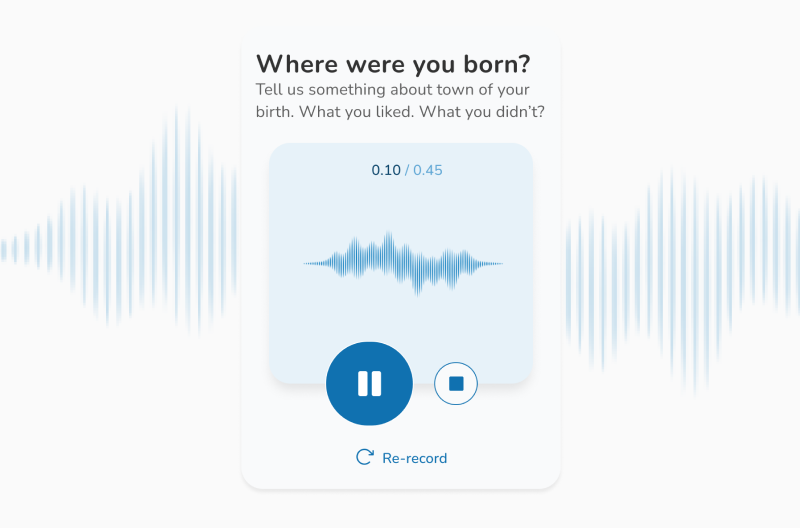
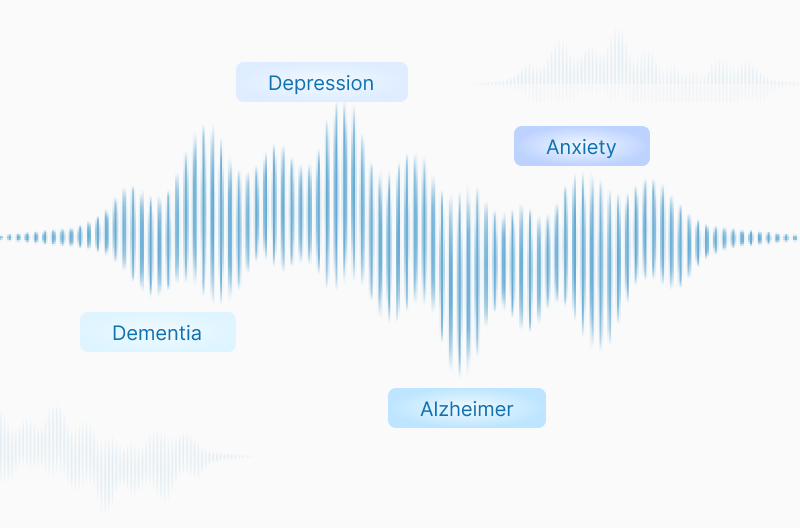
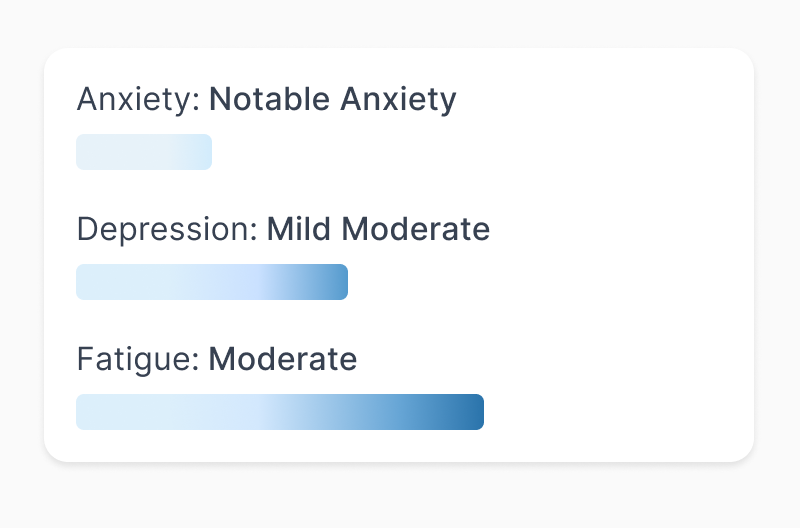
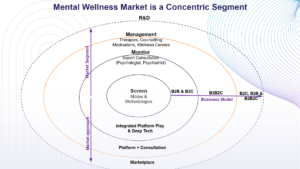
Yes! Over 150 million people in India suffer from disorders related to mental fitness, reflecting a substantial public health challenge. According to the National Mental Health Survey by NIMHANS, about 10.6% of adults in India suffer from mental disorders, and the lifetime prevalence reaches 13.7%—approximately 1 in 7 people require mental health interventions today. The biggest hurdle remains the stigma and taboo surrounding mental illness, which restricts open conversations and timely care. While Gen Z and younger generations are more open to addressing mental health, older generations still face deep-seated stigma and misunderstanding. The scale is massive, and the barriers are strong, making existing programs and systems insufficient to meet the need. The mental awareness market segment in India functions like a concentric ecosystem where various layers coexist and support each other. This interdependency is critical to building an end-to-end platform that advances research and development in precision psychiatry and neurodegenerative remedies. Like other emerging industries such as fintech and agritech, mental wellness is rapidly evolving, marked by technology fragmentation yet immense opportunity. Technology-driven advances in deep tech, AI, and democratized digital access, especially via voice and facial recognition, are transforming screening and monitoring paradigms. Wellness fundamentally depends on deciphering the complex, ever-changing state of mind. In today’s Volatility, Uncertainty, Complexity, and Ambiguity (VUCA) world, an individual’s mental state is continuously exposed to stressors leading to fluctuating wellness. Resilience levels determine severity outcomes, and these mental patterns correlate closely with personality traits that may manifest as erratic behaviors or, in some unfortunate cases, result in severe adverse outcomes without awareness. Two major market drivers are emerging within wellness: Preventive care and management. Prevention in mental health is paramount in a VUCA environment—early screening, self-help modules, and guided consultations are becoming widespread. Over the past decade and especially accelerated by the COVID-19 pandemic, preventive adoption has strengthened considerably. Awareness increased through government programs like the National Tele Mental Health Programme (Tele MANAS), which as of 2025, set up 53 cells across 36 States and UTs, answering over 2 million calls in 20 local languages, reflects a digital shift enhancing accessibility. Key segments include: Screening and Diagnosis: This is the critical entry point largely driven by self-reported and professionally guided questionnaires, followed by clinical validation. Innovations such as voice and facial recognition screening tools, powered by AI and edge computing, are pioneering more efficient and accessible diagnostic routes. Although clinical efficacy validation is ongoing, integrated tech stacks incorporating these tools provide promising avenues to overcome accessibility barriers. Monitoring: WHO guidelines recommend psychiatrists and psychologists for monitoring, but India faces a severe shortage with only 0.75 psychiatrists per 100,000 people (WHO recommends 3). This shortage, coupled with stigma, creates a dire gap in care—especially for progressive cases requiring active management. Digital ecosystems and on-demand consultations are evolving as critical solutions. Data-driven, platform-integrated models can improve prioritization, mobilization, and effectiveness in patient care. Management: The largest sub-segment, driven by rising stress and anxiety among working professionals, includes traditional wellness practices such as yoga and philosophies inspired by guru’s, alongside app-driven wellness programs featured in employee welfare. Given the highly individualized nature of mental health management, customer satisfaction and retention present unique challenges, with acquisition costs and ROI being significant business concerns. This segment is where science meets art, with an increasing role for technology-human hybrid models. Central to these segments is data and computational advances capitalizing on research & development across the wellness ecosystem. This includes advisory roles, governance frameworks, compliance, and validation led by academic and healthcare institutions, government bodies, and special purpose vehicles. With mental health contributing to significant disability-adjusted life years (DALYs) and high economic loss (estimated USD 1 trillion in India from 2012-2030), investing in these ecosystem roles is critical to sustainable impact. As we confront a global mental health crisis impacting over one billion people worldwide, the urgency to rethink and rebuild mental wellness ecosystems on a strategic level has never been greater. Mental health disorders such as anxiety and depression are leading causes of disability and substantial economic loss, costing the global economy an estimated $1 trillion annually. Despite increased awareness and some progress, stigma, underfunding, and workforce shortages continue to restrict access to quality care. The future demands bold, cross-sector collaboration and innovation—leveraging advances in digital health, artificial intelligence, and data-driven precision psychiatry—to democratize mental wellness globally. Mental health care must be recognized not as a privilege but as a fundamental human right, integral to social and economic well-being. The strategic challenge lies in transforming fragmented systems into holistic, accessible, and sustainable ecosystems that prioritize prevention, timely diagnosis, effective monitoring, and personalized management. Key strategic imperatives for the future include: Scaling access to care globally through telehealth, AI-driven diagnostics, and community-based interventions. Combating stigma by embedding mental health literacy in education, workplaces, and public campaigns. Expanding and upskilling the mental health workforce to meet growing demand and improve quality of care. Integrating mental health into primary health systems for early detection and holistic wellness. Leveraging data and technology for precision screening, real-time monitoring, and personalized treatment. Promoting multi-sector collaboration among governments, private sector, academia, and civil society. Prioritizing prevention and resilience-building strategies to reduce the overall mental health burden. Ensuring equitable funding that reflects mental health’s critical role in overall health and productivity.